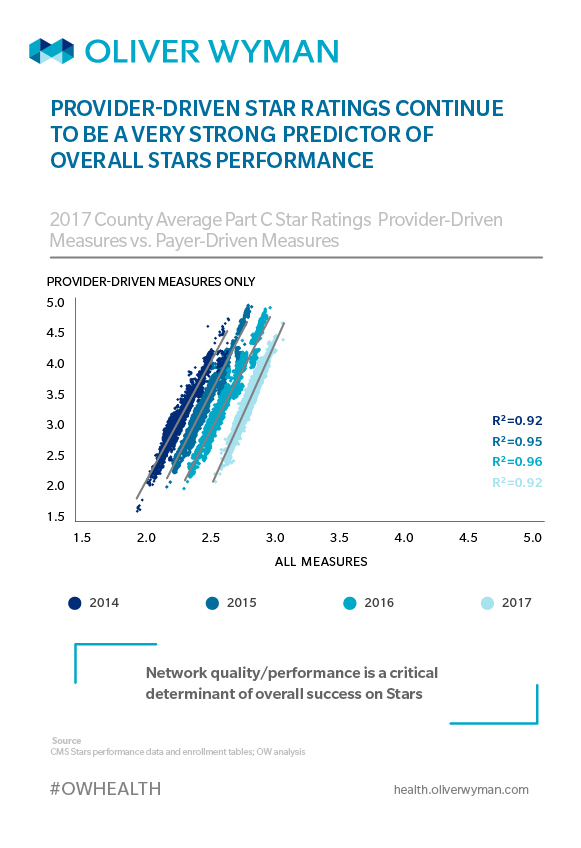
Editor’s Note: This piece is part of an ongoing series. In a previous article (Winning on Stars: It Starts and Ends with Providers), we discussed the importance of underlying provider network performance in driving a plan’s overall Stars score. 2016 Star year analysis showed overall score was highly correlated with performance of a plan’s contracted provider network, with an R2 of 0.95 – near perfect correlation. In a future post, we’ll consider the program changes required to raise a plan’s score from 3.5 Stars to 4.
Plans have continued to mature in their approach to Stars. Over the past two years, they have become more effective and more efficient at driving high quality scores overall, demonstrated by significant increases in the 4-Star thresholds of key measures. Despite this maturing of Stars programs, however, the dependency on underlying provider performance remains very strong.
Our analysis of annual Stars metrics demonstrates a continued high correlation between a plan’s overall Stars score and their performance on provider-driven measures.
While many plans have significantly improved their performance on internal, plan-driven measures of member experience and satisfaction, there is a need to focus greater efforts on the two-thirds of measures that are largely or entirely in the provider network’s control. Although the majority of plans manage to achieve 4- and 5-Star ratings on plan-driven measures, many still fall short on their overall ratings due to a lack of emphasis on engaging their provider network more assertively to close care gaps.
A comparison of county-level performance of plans at an overall Stars level versus the underlying county provider performance data makes clear provider network quality drives Stars performance.
This is not just an analytics exercise; plans that want to improve their Stars performance need to address underlying issues with their service area providers. In counties where underlying provider performance is strong, plans can count on provider engagement and gap closure to help achieve their objective. However, in areas where underlying provider performance has been sub-par, plans often end up over-indexing on member engagement, education, and incentives when trying to improve Stars performance.
But plans in these areas need to think more strategically about their Stars approach. If the provider network is critical to managing cost of care and providing superior outcomes, then it’s also critical to achieving high Stars scores. Plans need to change their thinking about Stars and start looking at network design, contracting, incentives, and sculpting as powerful tools in their Stars toolbelts. A plan is more likely to achieve 4 Stars by using these tools alongside traditional measure-level interventions.